
Training ABA Staff Efficiently
- Payam Moghaddam
- August 1, 2023
- 08 Mins read
- Training,Supervision
If you are reading this and you are an ABA professional, I don’t need to convince you of the importance of training. Nor do I need to reiterate the effectiveness of Behavioural Skills Training (BST). Yet I bet you’ve experienced subpar training at some point, and may even be struggling to find time to train others to the standard you want. How come? How can ABA practitioners be experts in teaching, yet struggle with providing expert training? Probably because it is not easy to train.
Training may be a simple concept to grasp, but simplicity is not synonymous with being easy. It’s not easy because training has lots of important organizational and follow-up aspects to it that can quickly overwhelm an already busy practitioner. With too much to manage at once, client care will take priority, and training will become to “tomorrow’s problem”.
So what can we do about it? How can we reduce the overhead and make training routine and systematic?
Why is Training Hard?
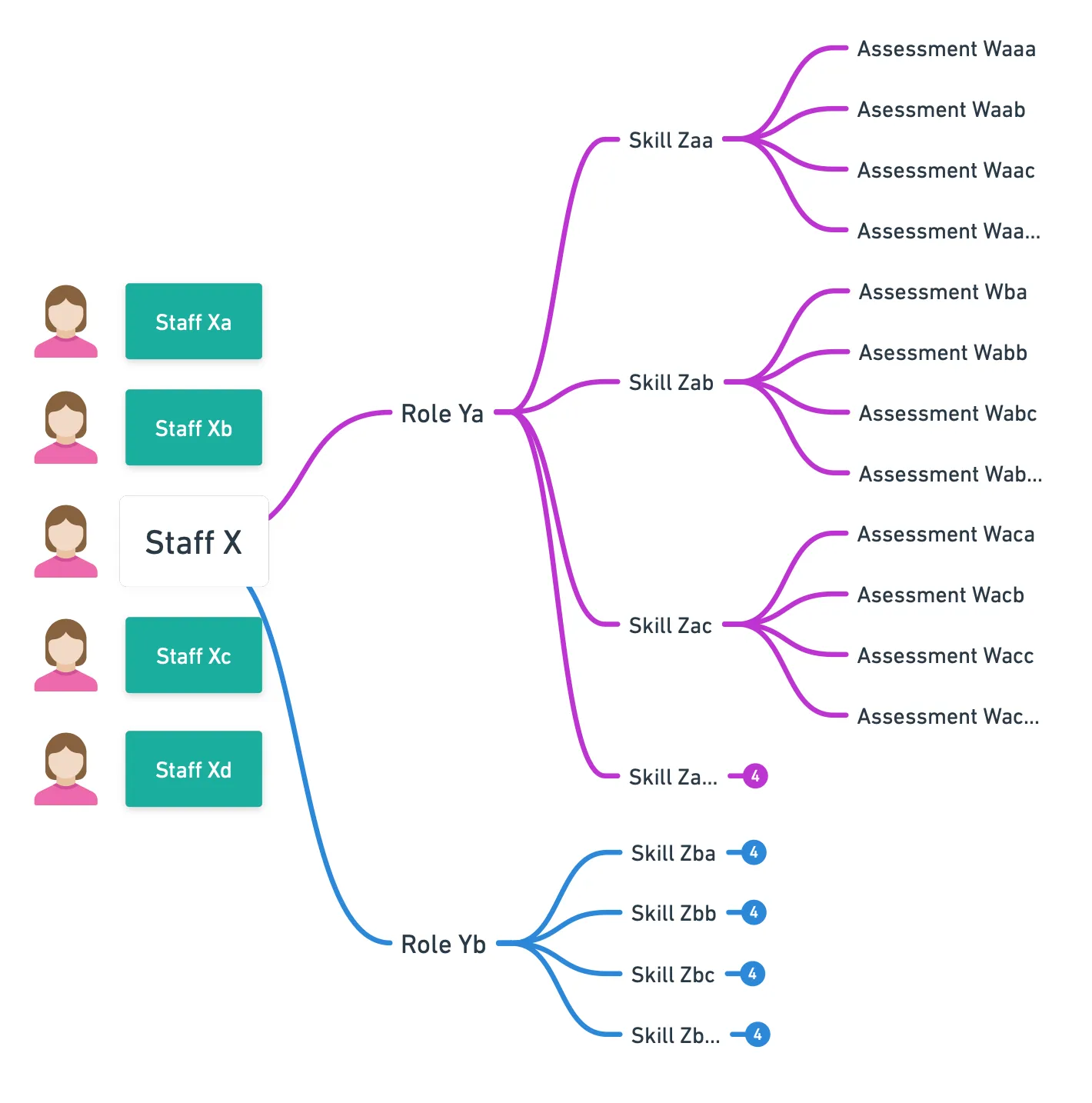
The most effective form of training is individualized training, using a curriculum that bridges the gap between a person’s existing competency and their expected competency. Unfortunately, for training to be individualized, you must be able to answer the following questions for each individual:
- What are the skills expected of individual X in their role Y?
- When did X get supervision and feedback for skill Z as part of role Y?
- Is X progressing, stagnating, or regressing on skill Z?
- What skills in role Y has X not been assessed against?
- Does X have clarity on what is expected of them and how they are doing so far?
These questions multiply as your staff grows (X), roles increase (Y), role assignments multiply (XY), and your skill matrix becomes better defined (Z per Y).
Even with answers to these questions, executing a training plan for each individual against their learning preference is a daunting task.
- How can I teach X based on their personal preferences and existing competency?
- How can I setup a supervision for X based on Z skills and notify them ahead of time?
- How can I track when was the last supervision for X so I don’t forget to support them?
- How can I make sure X receives the appropriate supervision follow-up and feedback?
It’s no surprise then, that despite a strong belief in training and knowledge of the BST model, majority of teams and clinics struggle to implement high quality training for their staff. The overwhelming organizational level of providing individualized, skill-based training, causes clinics to fallback onto a less adequate approach of generalized role-based training which often focuses on pivotal skills and hopes individuals can generalize them to their day-to-day practice. Furthermore, if clinics have to resort to generalized training, then they might as well leverage external training, which further diminishes the effectiveness of training since the content is no longer specific to their environments.
To overcome this negative cascading effect, we need to consider how to minimize the organizational overhead and design day-to-day tasks such that training is embedded into them, rather than separate to them.
Separate vs. Embedded Training Models
One way to think about training is to consider how many “hops” away from client care it is. If you see training as
We train people → so they can implement programs effectively → so clients benefit
Then training will always be seen as a “supporting” element rather than an “essential” element. Even if mandated by BACB’s Ethics Code, how we view training impacts our emphasis of it. And once you layer on financial incentives, lack of time and staff, you can see how contingencies align to deprioritize training.
Instead, consider training as:
People are trained as part of program implementation → so clients benefit
The training is now an “essential” part of program implementations, which naturally makes it more seamless as well.
Separate Training Model
If training is viewed as a separate task, then the contingencies encourage “standardized/group training material”, general 1-on-1 meetings for feedback, and “good enough data” for performance tracking for legal purposes. In such a system, staff are encouraged to train on their own, supervisors may lack time to provide granular feedback, and individual’s competencies is not centrally tracked. Our primarily understanding of staff becomes their role, rather than their skills, and as such assign cases primarily by role.
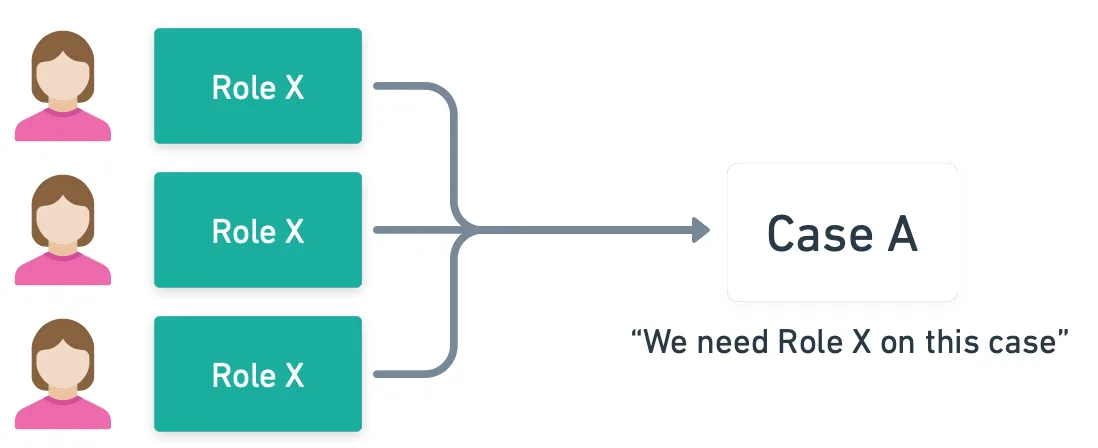
Embedded Training Model
If training is embedded into program implementations, individuals will be assigned to programs only if they have demonstrated competency for the skills required. As such, to assign individuals to clients and teams, supervisors work together to aggregate their skill assessments on staff into a common system for centralized visibility. As a result, in each supervision session or 1-on-1 meeting, everyone is incentivized to discuss addressing their skill deficiencies, prioritize gaining skill mastery since it influences their caseload, and everyone understands that clinic supervisors have clear centralized oversight on their performance level.
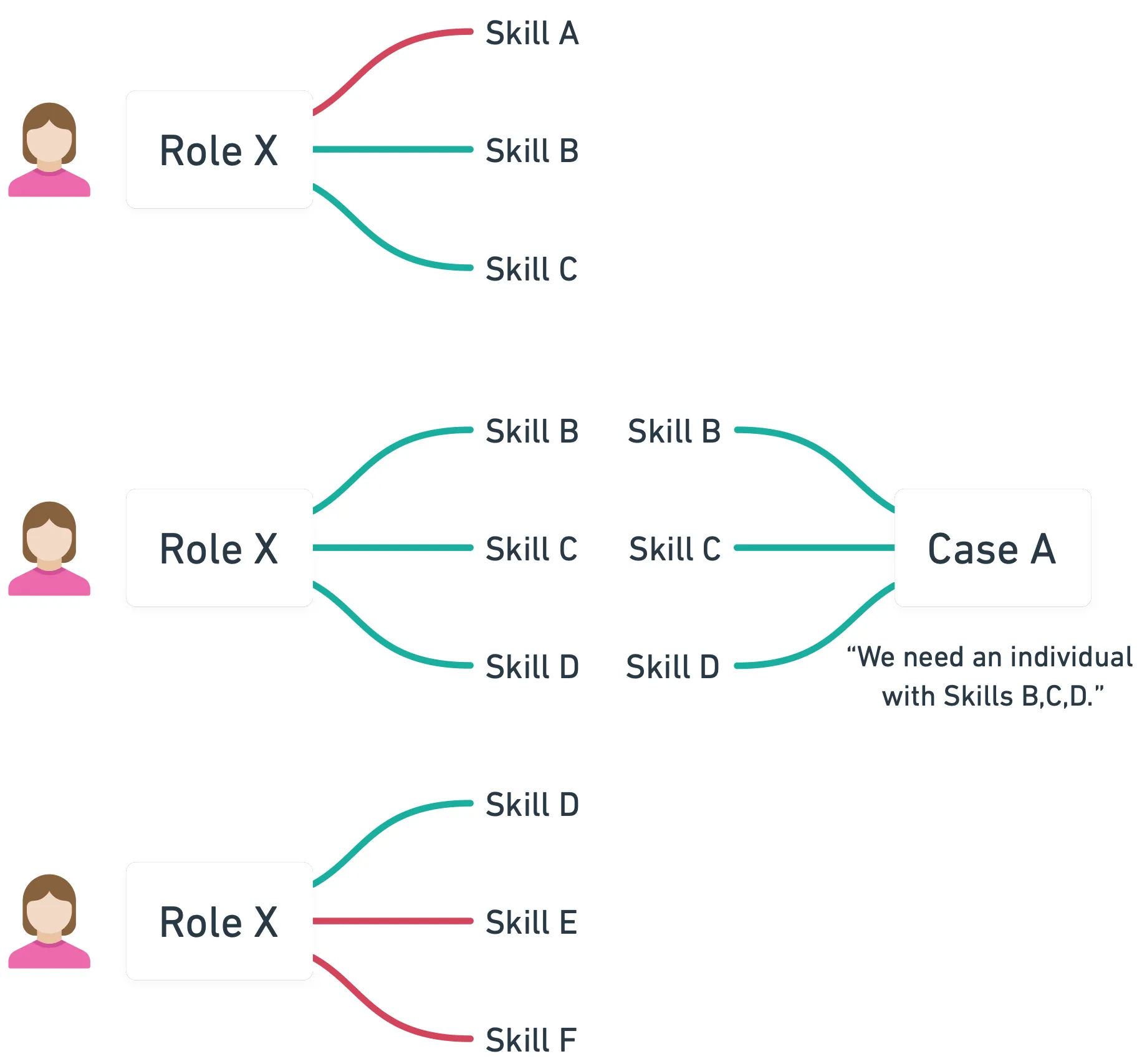
In this embedded model, training is not a distinct task, it’s a necessary task as part of case assignment.
You may notice though that this embedded approach has a dependency on a “system” to facilitate this. A system that automates the tracking overhead and provides centralized reporting visibility. How would such a system look like?
Key Components of Embedded Training
There are three distinct pieces required for embedded training:
- Role-based Skill Competency Matrix - you and your staff need to know what is expected of them in their roles.
- Individualized Skill Competency Tracking - a mechanism needs to exist to assess staff against skills in their roles and to track the results of these assessments.
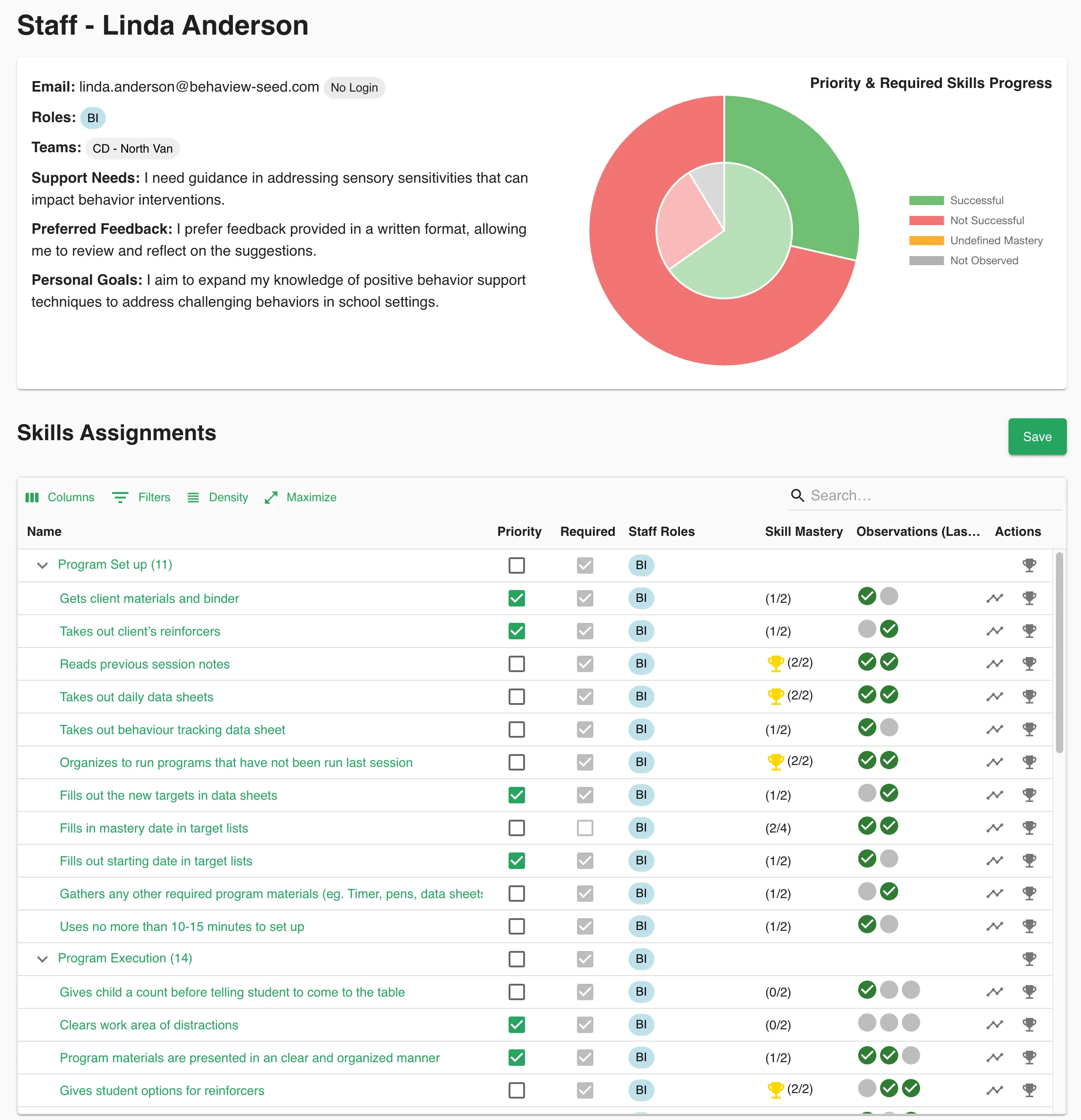
- Automated Reporting on Individuals’ Progress and Gaps - various views of individuals’ performance needs to exist so that individuals understand how they are performing, and for supervisors to understand what to prioritize for supervisees.
You want to be able to access a single view that visually informs you of an individual’s competency. The following is an example of how it can look like, and how it quickly helps you understand a staff member’s competency, per skill, with traceable visibility to past sessions. With this insight, you know what to prioritize next for them, and what cases and teams they’d be successful on. In fact, they will know what to prioritize for themselves!
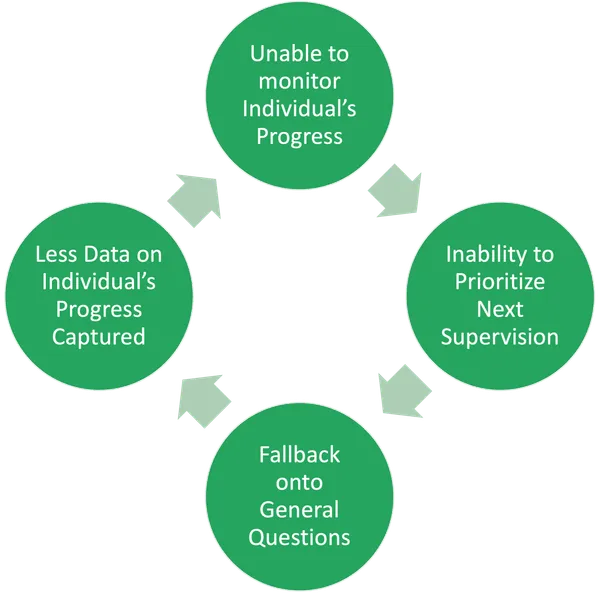
Typically, organizations get a few pieces correct, but without all the pieces to create a centralized view of each staff, organizations drift back to ad-hoc management and inevitably to separate training mechanisms. For example:
- you may know what you want per role
- you may regularly take supervision notes
- but you lack a way to aggregate those notes into a report
- so you struggle to know what to prioritize for the next supervision
- so you start prioritizing off of memory or simply your last supervision notes
- which you start finding not as effective as simply asking supervisees “What do you want to focus on today?”
- and thus you become reinforced to stop taking supervision notes since you don’t use them
- and eventually you fade out your training system and fallback on external training mechanism
Dedicated ABA Training Systems
Majority of software solutions today cater more to Human Resource (HR) professionals than to ABA professionals. Unfortunately, HR professionals are not well-versed in the science of learning like ABA professionals are, typically have various other responsibilities (e.g., employment contracts, local compliance laws, firing and hiring, etc.), and are almost never the experts who would supervise or train staff directly. As a result, majority of existing Human Resource Management Systems (HRMS) end up focusing more on tracking employees’ personal information, as well as their pay and sick days, with only minimal management capabilities (e.g., a basic 1-on-1 template for meetings). Such systems rarely (if ever) meet the needs of an ABA professional’s training standards and thus enthusiastic ABA supervisors tend to rely on DIY solutions built on spreadsheets and Word documents instead.
We built Behaview to address this gap. Emphasizing ABA principles first, then layering on staff management capabilities, leads to a stronger training and supervision system for ABA providers. And when supervisors can offload their organizational overhead to such a system, they can focus on the quality of the supervision itself and embed training into their day-to-day practice.
You can use the following evaluation criteria to assess your system today, and what to consider when either building or buying a new system.
| Capability | DIY Solution | HRMS | Behaview |
|---|---|---|---|
| Role-based Skill Competency Matrix | |||
| Scheduling of Supervisions and 1-on-1s | Typically limited to basic scheduling | ||
| Multiple Roles per Individual Support | Complicated to do via spreadsheets | Typically assume one role per person | Individuals can have multiple roles |
| Individualized Skill Mastery Tracking | A sheet per staff can work, but keeping it in sync with the skill matrix will be manual | You can see complete skill history per individual | |
| Automated Reporting on Skill Gaps | You can create charts off of your spreadsheets | Majority do not enable this, but some do | Visual reports and recommendation engine let you identify gaps quickly |
| Integrated BACB Supervision Fieldwork Tracking | A separate spreadsheet altogether will be needed | HRMS tools are not catered for ABA use | Fieldwork tracking is built-in with BACB Task List support too |
| Mobile & Tablet Support | Excel can be accessed on phone, but no one will say it is “convenient” | Modern HRMS may have a simplified mobile UI | You can use Behaview on any device with an optimized UI |
Permission Controls to Enable Oversight by Clinical Supervisors and Directors | Complex to do but permissions can be managed per spreadsheet | Typically only direct reporting hierarchy is supported | You can assign permission to reporting hierarchy or groups of individuals |
If you have no system in place today, it’s worthwhile having a conversation as a team and aligning on the sort of training you all want. Through team conversations you’ll better know what sort of solution is suited for you and your team, and you’ll have team buy-in for its successful adoption.
Efficiently Applying the Science of ABA
Training is critical and something ABA providers do on a daily basis, but scaling effective training, while maintaining full caseloads, is not easy. A focus on efficiency and baking training into day-to-day processes helps to ensure its consistent practice rather than it becoming “yet one more thing” everyone has to do. It certainly requires taking a step back to re-evaluate existing processes and how to leverage modern tools to reduce the overhead. But once it’s done, training will become automatic and it’ll be one of the greatest factors in your staff’s retention and happiness, including your own!